The Science Blog

AI in Personalised Medicine: Opportunities and Challenges
Recently, Artificial Intelligence (AI) has changed healthcare. This is especially true for personalised medicine. This convergence will change patient care. It will customise treatments based on each person’s genes, environment, and lifestyle. But, like any new technology, this journey has both chances and obstacles. In this exploration, we will look at how AI is changing personalised medicine. We will also discuss the challenges we need to overcome to reach its full potential.
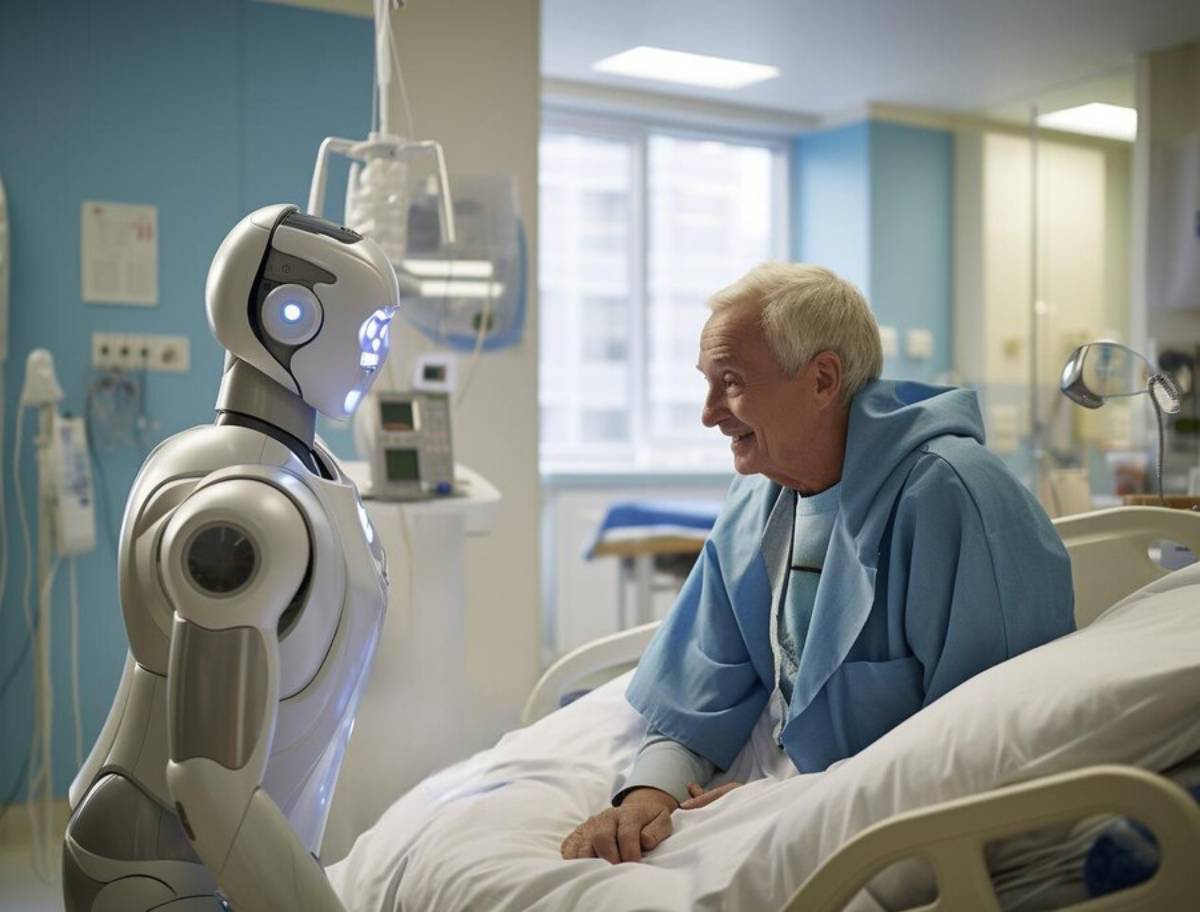
AI healthcare, with its predictive diagnostics capabilities, is heralding a new era of medical practice. However, misconceptions abound, particularly regarding the safety and efficacy of AI-driven approaches. Many fear that the reliance on algorithms could overshadow the human touch in healthcare. When used wisely, AI can enhance healthcare professionals’ skills. This leads to better and more effective patient care.
Key Benefits of AI in Personalised Medicine
Transforming Patient Care
AI can analyse large datasets quickly and accurately. This skill greatly impacts personalised medicine. AI healthcare tech helps medical professionals find patterns and connections that were hard to see before. This ability is especially useful in predictive diagnostics. AI can spot potential health issues before they appear. This helps with early interventions.
AI analytics can analyse various data sources. This includes electronic health records (EHRs), genomics, and wearable health devices. These insights help clinicians make smart choices. They improve diagnostic accuracy and allow for interventions that fit the patient’s unique biology. The shift from reactive to proactive care is a defining feature of AI-enabled personalised medicine.
Enhancing Treatment Precision
Personalised medicine thrives on the principle of tailoring treatments to individual patients. AI is key here. It analyses genetic information. This helps predict how patients will respond to certain treatments. This precision cuts down on the trial-and-error methods often used in medicine. As a result, patients recover faster and have better outcomes.
In pharmacogenomics, which studies how genes influence drug responses, AI can predict bad reactions or ineffective prescriptions. Using these insights in treatment planning can help healthcare providers lower hospital readmissions and boost treatment effectiveness.
Real-Life Applications
One of the most promising applications of AI in personalised medicine is in oncology. AI algorithms can analyse tumour samples to find genetic mutations. This helps oncologists choose the best treatment plans. AI helps predict how patients will respond to chemotherapy. This reduces side effects and improves their quality of life.
Other uses are AI-guided imaging analysis in radiology. Here, machine learning models help find abnormalities accurately. In neurology, AI tools help personalise treatment for disorders like epilepsy and multiple sclerosis. They track disease progression and therapy responses over time.
Data-Backed Insights
The integration of AI in healthcare is backed by robust data. A study in The Lancet showed that AI can predict breast cancer risk up to five years early. This method is more accurate than traditional ones. These insights show how AI can transform predictive diagnostics and personalised medicine.
A recent study from Stanford University showed that AI can spot genetic disorders in newborns with rare diseases in just a few hours. This is much quicker than the weeks needed with traditional genomic methods. These advances lead to quicker diagnoses and early treatments. This is crucial for handling complex or urgent health issues.
Additional Expert Tips & Common Mistakes to Avoid
Best Practices in AI Healthcare
To harness the full potential of AI in personalised medicine, healthcare providers must adhere to best practices. This means keeping data private and secure since patient information is sensitive. Also, ongoing training and education for healthcare workers are key to keeping up with fast tech changes.
Effective collaboration between clinicians, data scientists, and IT professionals is essential. Medical staff should be involved in the AI tool development process to ensure usability, relevance, and trust in the results. Institutions should focus on the transparency and the explainability of AI models. This helps them keep ethical standards and follow regulations.
Avoiding Common Pitfalls
Despite its potential, AI healthcare is not without its challenges. One common mistake is over-reliance on AI without human oversight. AI processes data very quickly, but it doesn’t understand things like humans do. Therefore, AI should be viewed as a tool to assist, rather than replace, human judgement.
Another challenge is the presence of algorithmic bias. AI systems need diverse data for accurate results. Without it, they can create skewed outcomes, especially for underrepresented groups. To tackle bias, we need to collect inclusive data and regularly check how AI performs for various demographic groups.
Misconceptions and Their Impact
A prevalent misconception is that AI will lead to job losses in the healthcare sector. However, AI is more likely to create new roles, particularly in data analysis and AI system management. By tackling these misconceptions, the healthcare industry can get ready for AI technology integration.
Instead of replacing clinicians, AI is expected to shift their roles. This allows them to focus on complex care tasks while automating routine processes. This evolution will enhance workforce efficiency and free up time for direct patient engagement.
Advanced Insights / Expert Recommendations
Navigating the Ethical Landscape
The ethical implications of AI in personalised medicine cannot be overlooked. We must tackle issues like data privacy, consent, and algorithmic bias. This is key to making AI healthcare solutions fair and just. Experts say we should set clear ethical guidelines. It’s also important to involve different stakeholders when developing AI technologies.
Patients must have the right to understand how their data is being used and to provide informed consent. Regulatory frameworks like GDPR in Europe help manage data rights. However, organizations need to do more to build and keep patient trust. Ethical AI means checking systems for bias often. It also includes using feedback loops to improve performance.
Industry Perspectives
From an industry standpoint, collaboration between tech companies and healthcare providers is essential. By teaming up, these groups can create AI solutions that are advanced and useful in a clinical setting. This partnership helps share best practices and lessons learned. This speeds up the use of AI in personalised medicine.
Pharmaceutical companies are using AI to make clinical trials faster. They also find new drug targets and repurpose existing drugs. These partnerships are critical to translating AI research into real-world health benefits.
Lesser-Known Insights
A lesser-known aspect of AI in healthcare is its potential to democratise access to personalised medicine. AI lowers the cost and time of medical research. This makes personalised treatments easier for all patients. Now, access is better, no matter where they live or their financial situation.
AI-powered telemedicine platforms allow remote consultations and diagnostics. They help close the healthcare access gap in underserved areas. AI translation tools are boosting global communication between patients and providers.
Final Thoughts: Embracing the AI-Driven Healthcare Revolution

AI is set to change personalised medicine. It will boost patient care with better diagnostics and customised treatments. To gain these benefits, the healthcare industry must overcome many challenges. These include ethical issues, regulatory rules, and the need for human oversight. Using AI as a helpful tool can lead to better health outcomes. Tackling these challenges directly makes this potential even greater.
We are at the start of a new era in medicine. It’s crucial for healthcare providers, policymakers, technologists, and patients to join forces. Together, we can make AI-driven personalised medicine a reality, not just a dream. It requires a collective effort, a clear vision, and an unwavering commitment to ethical innovation. The future of healthcare is smart, personalised, and AI-powered—are we ready to seize it?









